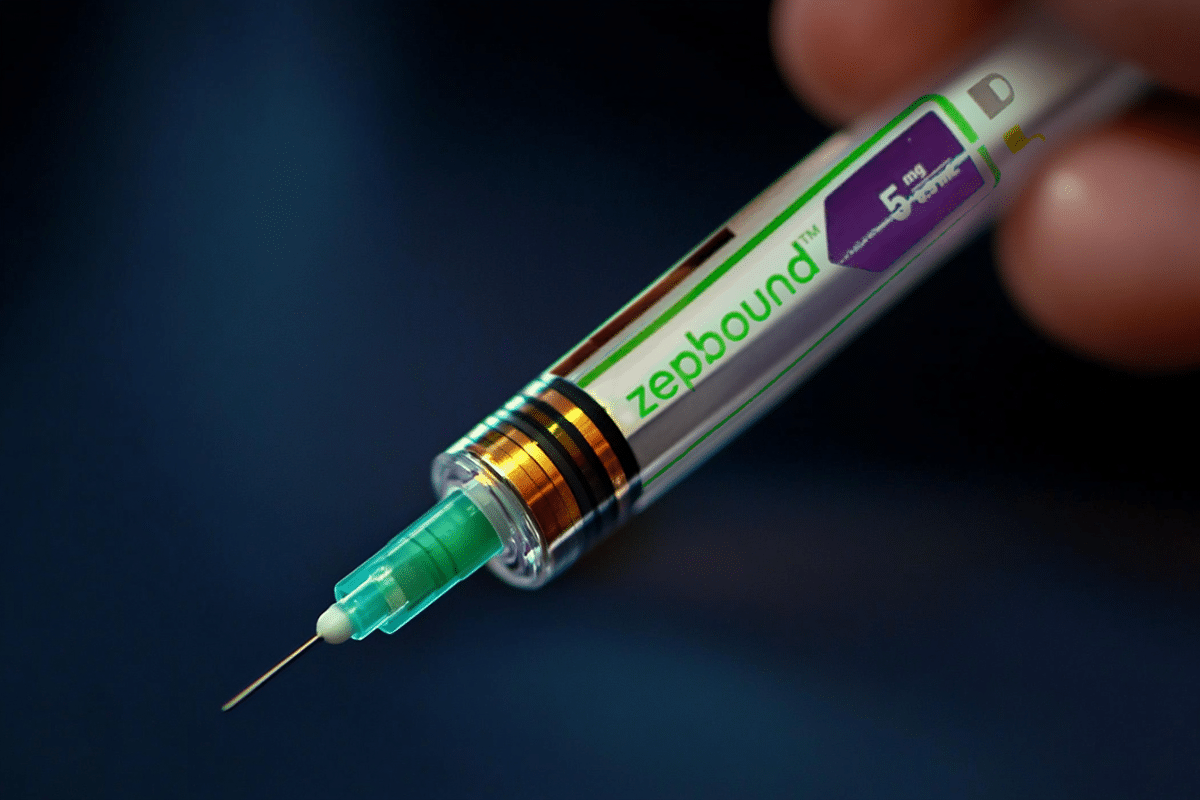
The demand for weight loss medications in the United States has skyrocketed in 2024, with prescription fills for Wegovy and Zepbound more than doubling. These drugs, part of a category known as GLP-1 and GIP agonists, regulate appetite and blood sugar by mimicking gut hormones. Their growing popularity underscores the persistent demand for these treatments, despite challenges related to affordability and access.
Zepbound, a recent addition to the market approved in November 2023, saw prescription fills increase by over 300% in its first year. Wegovy, approved in 2021, recorded a more than 100% rise in prescriptions since the start of 2024. Both drugs carry hefty price tags of around $1,000 per month without insurance or discounts.
While these medications offer transformative weight loss solutions, many Americans struggle with the financial burden. Insurance coverage for these drugs remains limited, with just 9% of commercially insured patients enjoying unrestricted access to Zepbound and 14% to Wegovy. A significant portion, between 60% and 70% of patients, face restrictive coverage conditions, such as prior authorizations or higher BMI thresholds. Alarmingly, nearly 20% of individuals with commercial insurance lack coverage for at least one of these drugs.
For insured users, out-of-pocket costs can still be substantial. Zepbound users pay over $2,500 annually in copays on average, with monthly costs averaging $231 in 2023. For the uninsured, tools like GoodRx offer some relief, saving users up to $250 per month or $3,000 annually. Despite these options, many Americans have overspent an estimated $200 million by paying full retail prices instead of leveraging savings programs.
The demand for these drugs is not only a testament to their efficacy but also highlights gaps in healthcare accessibility. Less than 20% of large employers in the U.S. provide health insurance plans that include coverage for weight loss medications. Medicare does not currently cover such treatments unless they are prescribed for another health condition, further limiting access for older adults and other vulnerable populations.
Recent policy proposals aim to address these gaps. In November, the Biden administration suggested expanding Medicare and Medicaid coverage for weight loss medications prescribed to patients with obesity. If implemented, this change could significantly improve access, though it may also raise costs for employers, state governments, and federal programs.
As these medications grow in popularity, the focus on their affordability and accessibility is intensifying. Although tools like GoodRx provide significant savings for many users, they cannot fully replace the advantages of comprehensive insurance coverage. The rising demand highlights an urgent need for improved policies that ensure these groundbreaking treatments are available to those who need them the most.