In a significant stride for infectious disease diagnostics, researchers have developed a novel technology capable of accurately differentiating between Zika and dengue virus infections. This advancement is particularly vital in regions where both viruses are endemic, offering hope for improved treatment strategies and vaccine development.
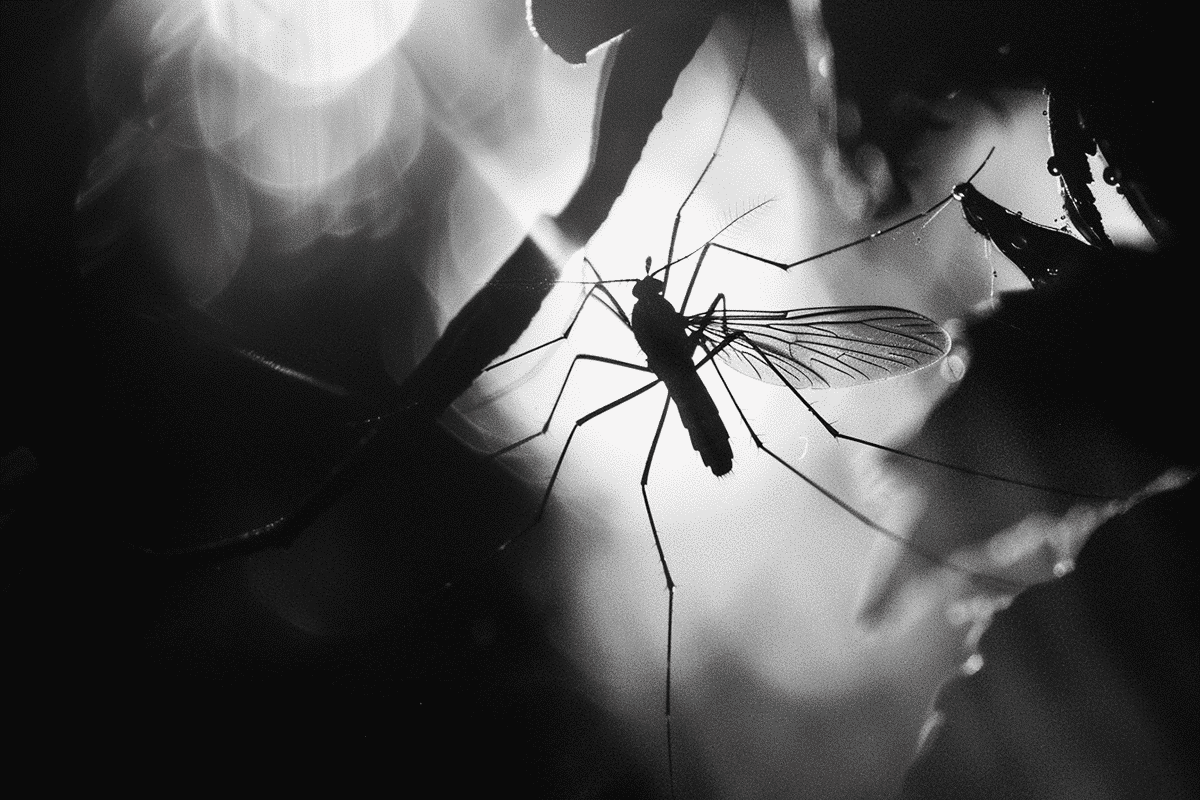
The Zika virus, recognized for its rapid spread to the Americas in 2015, is primarily transmitted through mosquito bites, similar to the dengue virus. Both viruses often result in the production of similar antibodies, which until now, have made it challenging for health professionals to accurately diagnose and differentiate between the two. This confusion can have serious implications, especially for pregnant women, as Zika infection during pregnancy is linked to significant birth defects.
Researchers at the University of Pittsburgh Public Health, led by Priscila Castanha, PhD, have utilized what they describe as “peptide-inspired conformationally constrained oligomers” (PICCOs) to tackle this diagnostic dilemma. These synthetic molecules are engineered to mimic the epitopes of pathogens, thereby attracting virus-specific antibodies.
The team’s method involves screening half a million PICCOs against blood samples from individuals known to have been infected with either Zika or dengue. Through this extensive screening, they identified 40 PICCOs that reacted specifically with Zika virus antibodies. Notably, one PICCO, labeled CZV1-1, proved particularly effective, correctly identifying Zika infections 85.3% of the time while maintaining a low false positive rate of only 1.6%.
This technology marks the first use of epitope surrogate technology in the fight against Zika. It addresses a crucial gap in the current diagnostic tools available for differentiating infections within the flavivirus family, which includes not only Zika and dengue but also other mosquito- and tick-borne viruses.
One of the most groundbreaking aspects of this new technology is its practicality in field conditions. The PICCOs do not require refrigeration, a common challenge in many tropical regions where these viruses are prevalent. This attribute makes the technology an invaluable asset for remote or resource-limited settings, enhancing the capacity to manage and control outbreaks effectively.
The development of this diagnostic tool is not just a technical achievement but also a logistical one, simplifying the testing process significantly. During the Zika outbreak in 2015, accurate diagnosis was cumbersome and required multiple tests to confirm infection. The introduction of the CZV1-1 PICCO could streamline this process, reducing both the time and resources needed to diagnose Zika virus accurately.
The implications of this technology extend beyond immediate diagnostics. By providing a reliable means to distinguish between Zika and dengue infections, health authorities can better assess immunity levels within populations, improve clinical trials for new treatments, and enhance epidemiological studies. This could be particularly impactful in areas like Brazil, where large segments of the population have been exposed to both viruses.
Furthermore, the ability to differentiate between these infections accurately can inform public health decisions and potentially guide vaccine development, ensuring that resources are directed towards the most pressing health threats.
As this technology moves towards broader application, it promises not only to refine our approach to diagnosing and managing Zika and dengue but also to provide a template for responding to other viral outbreaks. This epitope surrogate technology, by offering a precise and adaptable diagnostic tool, represents a pivotal advance in the global fight against viruses transmitted by mosquitoes and ticks.